Is It Broken or Fractured?
Have you ever wondered what the difference is between a broken vs fractured bone? You may have even heard the words “fracture” and “break” used interchangeably. This is because fracture and break mean the same thing. A fracture (aka break) occurs when an outside force is too great for a bone to handle. Some may argue that the word “fracture” sounds gentler or more sophisticated than break. Regardless of the reason, “fracture” is the preferred term used by most medical professionals when describing a broken bone.
“‘Is it broken or is it fractured?’ is one of the most common questions we get asked by parents when dealing with pediatric ankle injuries in our practice. There isn’t a difference, but when polling patients and other doctors, ‘fracture’ seems to be the preferred term, both by medical professionals and parents alike,” explains Dr. Mark E. Solomon, D.P.M.; Foot and Ankle Surgeon at the Pediatric Orthopedic Center and director of the Pediatric Foot & Ankle Fellowship.
Ankle Injuries by the Numbers
Ankle injuries are the #1 sports injury and rank #2 for physeal or growth plate injuries. On average, 28,000 ankle injuries occur daily. The peak age for ankle injuries is between 8 and 19 years of age. Here at The Pediatric Orthopedic Center, podiatrist Dr. Mark Solomon sees about 4,500 to 5,000 ankle injuries per year, with ankle injuries accounting for both the number one pediatric sports injury and the most common physeal (growth plate) injury seen in his office.
Fracture vs Overuse Ankle Injuries
A stress fracture in the ankle is caused by overuse rather than sudden trauma, unlike other fractures. A significant factor contributing to ankle overuse injuries and stress fractures in children is the prevalence of year-round sports participation. Furthermore, early specialization in one sport can lead to overuse injuries due to repetitive movements. At our practice, we encourage children to engage in multiple sports and discourage joining two teams playing the same sport in one season. Additionally, it is advisable for kids to take breaks from training throughout the year and refrain from daily training. Stress fracture treatment typically involves avoiding weight on the injured bone while it heals and immobilizes the ankle with a cam brace. Rest plays a crucial role in the recovery process. When the time is right, your doctor may recommend physical therapy to strengthen the muscles around the injured bone.
Growth Plate Ankle Injuries
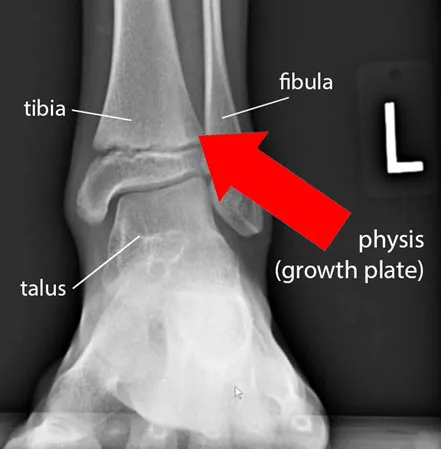
Children aren’t just small adults; their bones are still growing. The growth plate, known as the physis, is particularly vulnerable to extreme rotation, contortion, or abnormal movements. As children’s growth plates are open and more susceptible to injury, they can be more prone to a growth plate fracture and ankle injuries during their growth phase. Physeal ankle injuries often happen because children’s ankle growth plates are weaker than the surrounding ligaments and tendons, making them more prone to damage. These injuries typically occur in the tibia or fibula. The ankle joint is composed of the tibia, fibula, and talus. As children grow older and these bones fuse together, transitional ankle fractures may occur.
A broken ankle x-ray helps identify a growth plate injury, as depicted in the above image showing the widening of the ankle growth plate.
Transitional Ankle Fractures
During adolescence, when the growth plate in the ankle starts closing and hardening, transitional fractures can occur in the maturing growth plate. These fractures, seen in adolescents, occur when the growth plate has partially closed. Two common types of transitional ankle fractures are Triplane and Tillaux fractures, both caused by traumatic forces on the ankle joint.
A Triplane ankle fracture (Salter-Harris IV) involves the physis (growth plate), epiphysis (the rounded end of a long bone at the joint), and metaphysis (where the epiphysis meets the long bone shaft). On the other hand, a Tillaux fracture (Salter-Harris III) is an intraarticular fracture involving the physis and epiphysis, crossing the joint.
Transitional ankle fractures exhibit symptoms like inability to stand or walk, bruising, tenderness upon touch, and ankle area deformity. If you suspect your child has a transitional ankle fracture, it’s crucial to keep weight off the ankle and seek immediate medical attention.
Salter-Harris Classification Of Ankle Injuries
Salter-Harris fractures encompass a range of growth plate injuries occurring in children and adolescents, each categorized into different types based on the nature and location of the fracture. These fractures occur at the growth plate, known as the physis, and are crucial to understanding due to their implications for bone growth and development. The classification involves distinct Salter-Harris fracture types that delineate the specific characteristics and complexities of each fracture. An epiphyseal fracture, such as those in the Salter-Harris classification, may involve various presentations and treatments, each tailored to the unique nature of the injury. Let’s delve into the specifics of these fractures through a series of case studies and their respective treatment approaches.
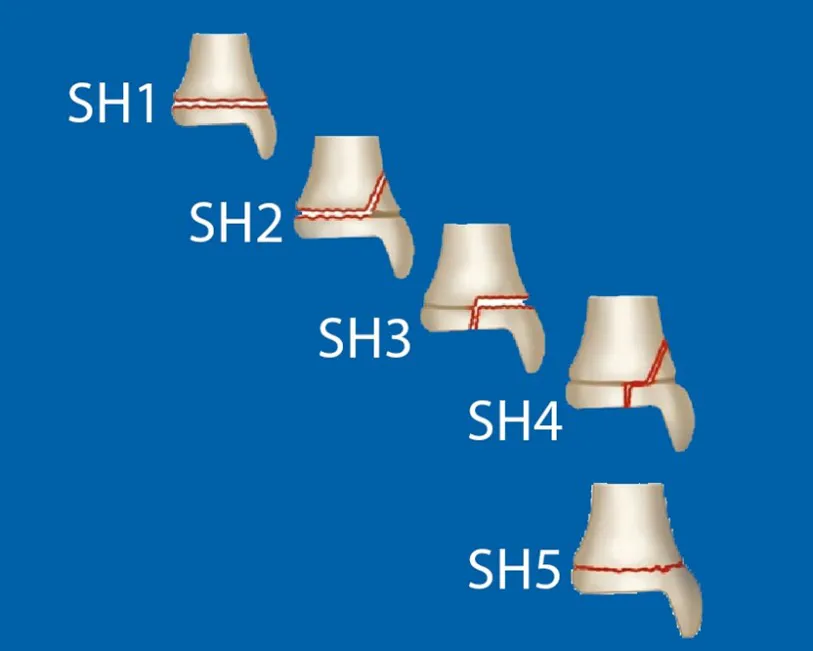
Fractures indicated in red show the relationship of fracture to growth plate for each Salter-Harris type
Salter-Harris Type I (SH1)
Salter-Harris I fractures occur across the level of the physis, separating the main part of the bone from the growth plate. Widening of the physeal plate is one of the most common observations with Salter-Harris I fractures. Children with a SH1 type fracture often present with ankle sprains and experience significant tenderness over the lateral physis. Typically, we don’t initiate treatment in the first 24-48 hours. Instead, we immobilize them short-term by placing them in a cam walker, allowing about a week for everything to settle. After this rest period, we schedule a follow-up in our office, transitioning them long-term into an ASO brace and commencing physical therapy. Consistent daily physical therapy exercises at home are crucial for a safe return to sports and to prevent chronic ankle instability.
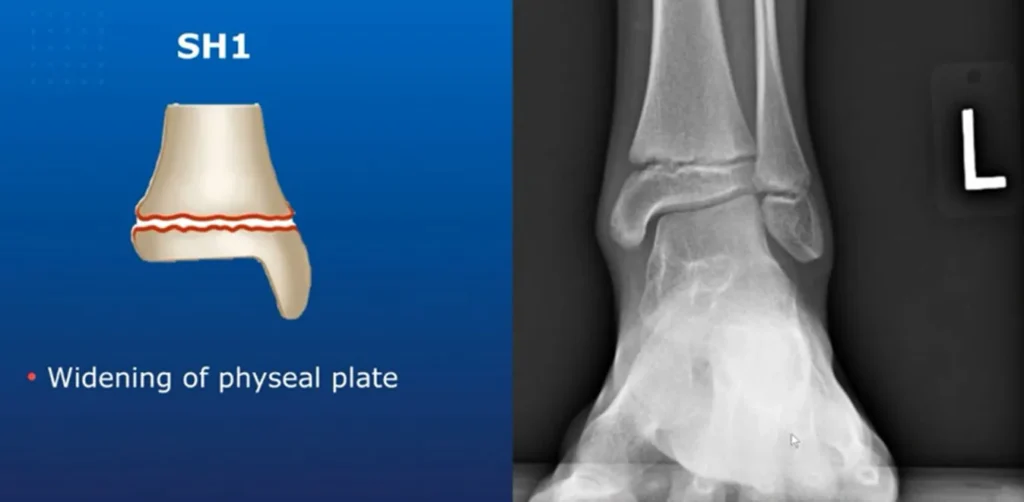
Case Study: Nine-year-old Soccer Player
The above X-ray depicts an SH Type 1 distal tip buckle fracture of the fibula in a 9-year-old male soccer player. The SH1 fracture resulted from a displaced tibia during a slide tackle while playing soccer. He was seen in the emergency room and treated with a temporary splint. Three months later, just before attending summer camp, he was placed in an AOS brace and able to attend camp.
Salter-Harris Type II (SH2)
Salter-Harris II fractures occur above the physis when the fracture extends through both the growth plate (physis) and the metaphysis, away from the joint space. These are the most common types of Salter-Harris fractures.

Case Study: Eleven-year-old Fall Injury
The above X-ray depicts an SH Type 2 fracture in an 11-year-old female. There was a delay in treatment while the patient was admitted to the hospital, and the cause of the fall from a 2nd-story window was investigated. The patient visited our office 2.5 weeks later with her foot stuck in an equinus position, a condition that limits the upward bending of the ankle joint. She was treated by splinting her in a plantar flexion position. However, she developed an Achilles ulcer, further complicating the case. Subsequently, she underwent a procedure in the operating room where the entire physis was reduced and brought back into alignment through manipulation. It was clamped together using a set of bio-lateral screws, eliminating any abnormal rotation.

Case Study: Nine-year-old Male Vitamin D Deficiency
The following X-ray depicts an SH Type 2 fracture in a 9-year-old male. The displacement was caused by a vitamin D deficiency. The patient was treated by immobilizing the ankle in a short leg cast for a period of two weeks before being transferred into a cam walker.
You may have heard the term ‘Thurston-Holland fragment’ used by your doctor. A Thurston-Holland fragment, also known as a corner sign, occurs when a small corner of the metaphysis is visible, as depicted by the dashed line in the above X-ray image.
Salter-Harris Type III
Salter-Harris III fractures occur lower into the epiphysis. These fractures extend from the joint surface through the growth plate into the metaphysis, which is the wider part of the bone. Salter-Harris Type III fractures account for 25% of all Salter-Harris fractures. The above x-ray image depicts an intraarticular fracture without anterior or posterior displacement. The treatment involved casting and immobilization for 4 weeks before transitioning the patient to a cam walker and beginning rehabilitation.
Salter-Harris Type IV (SH4)
Salter-Harris IV fractures occur transversely through the physis, extending across the bone, growth plate, and joint surface. These less common Salter-Harris Type 4 fractures require urgent orthopedic evaluation due to the risk of growth impairment, altered joint mechanics, and reduced functionality. Because these fractures involve the epiphysis, they may cause damage to the articular cartilage. An example of such a fracture is a Triplane ankle fracture, which consists of three components: a vertical component through the epiphysis, a horizontal component through the growth plate, and an oblique component through the metaphysis.

Case Study: Seven-year-old Male
The above X-ray shows an SH Type 4 fracture with slight displacement of the distal fibula, extending into the joint and medially into the physis. The patient underwent treatment in the operating room involving bio-integrative screws, along with a clamp and guide wire, to aid in reducing the physis.
Salter-Harris Type V (SH5) – Ruined
Salter-Harris V fractures occur when the growth plate is compressed or crushed due to injury. In Salter-Harris Type 5 fractures, the force at the time of injury is transmitted through the epiphysis and physis, potentially disrupting the germinal matrix, hypertrophic region, and vascular supply. As these rare fractures typically result from severe injury, they can have a poor prognosis, potentially leading to bone growth arrest.

Case Study: Eight-year-old Female
The above X-ray shows an SH Type 5 fracture that was initially mistaken for a potential bone cancer due to the razor line observed in the emergency room. The injury occurred during a hiking trip when both the patient and a family member tripped simultaneously, causing the family member’s shoulder to land on the patient’s ankle, resulting in a crush injury. After ruling out bone cancer, the patient underwent ankle surgery in the operating room with biomedical screws. Nine months post-operation, a small area of inter-physeal closure was noticed. The treatment plan involved waiting for three months to observe any further development of tethering, which was confirmed by a CT scan conducted at that time. This observation led to the decision for surgery to remove a portion of the bone block. This step was taken because the patient still has 3-4 years of growth ahead.
Ankle Fracture Complications
Ankle fractures in pediatric patients present unique challenges and considerations, often requiring tailored approaches for effective management. Complications can arise, especially in cases involving multiple manipulation attempts, where repeated adjustments can impact the delicate growth plates or lead to potential growth disturbances. Transitional ankle fractures, spanning the growth plate, demand careful attention due to their influence on the distal tibia and fibula physis. Premature physeal closure and distal fibula physis injuries, including Tillaux and avulsion fractures, necessitate precise evaluation to prevent growth plate issues and ensure proper healing. The complexities of a Triplan fracture, involving multiple planes of the growth plate, further emphasize the need for meticulous treatment strategies.
In instances of a broken ankle, especially concerning Tillaux fractures, the choice between operative and non-operative approaches remains a critical decision point in management. Non-operative treatment, involving casting or immobilization, might be suitable for smaller Tillaux avulsion fractures. Conversely, larger fractures or those with significant displacement may require surgical intervention to ensure anatomical alignment and promote optimal healing, reducing the risk of growth disturbances. This surgical approach often involves ankle surgery with screws to secure the fractured bones and facilitate proper fusion.
The Pediatric Orthopedic Center
The Pediatric Orthopedic Center is the premier NJ hub for pediatric orthopedics, with three offices throughout northern NJ and two pediatric-trained foot and ankle specialists. Having been the leader in pediatric orthopedics in this area for 30 years, we are the largest and most award-winning pediatric orthopedic practice in the tri-state area.



